|
The Role of Collagen
Crosslinking in the
Treatment of keratoconus and
Ectasia
Collagen crosslinking with
riboflavin (C3R) is a
relatively new procedure
that has been developed to
increase corneal rigidity
through increased
crosslinks.1-4 The procedure
has been shown to increase
corneal rigidity in both
porcine and human corneas in
experimental studies3 and
has been used in the
treatment of keratoconus,s>6
arresting collagen melts in
corneal ulcers7 and in
ectasia following LASIK.s
How does it work?
Riboflavin, or vitamin B2,
acts as a photomediator and
is absorbed by ultraviolet
light at 370 nm. Free
radicals are created, which
cause a change at the Amino
group of amino acids in
collagen. This change
results in an increase in
covalent bonds in corneal
collagen, leading to
thickening of colla-gen
fibrils and an increase in
tensile strength of the
cornea.
UVA light 370nm
The maximal effect of
crosslinking is confined to
the anterior 300 microns of
the cornea.
How is it performed?
The goal is to ensure that
riboflavin penetrates the
cornea, but as riboflavin is
a large molecule,
penetration through the
corneal epithelium is
difficult without either
removing or creating breaks
in the epithelium or by
breaking the tight junctions
between epithelial cells
through use of agents such
as tetracaine. There are
champions of both.
Riboflavin is instilled and
although advised to be used
every 5
minutes for 30 minutes, it
is absorbed into the cornea
with less frequent drops as
long as the eyes are kept
closed and patient is kept
supine. To ensure adequate
absorption, the eye is
checked at the slitlamp to
ensure the cornea is stained
yel¬low and the presence of
riboflavin is confirmed in
the anterior chamber.
Riboflavin with dextran is
used in corneas that are 400
microns or more in thickness
to avoid potential
endothe¬lial damage. In
thinner corneas, an
alternative preparation of
riboflavin without dextran
is used. The solution is
hypotonic and fluid is
absorbed into the cornea,
inducing some thicken¬ing.
This is checked using
pachymetry to ensure that
the cornea has thickened to
400 microns before
commencing UV radiation. A
speculum is inserted and
topical anesthetic is
applied periodically.
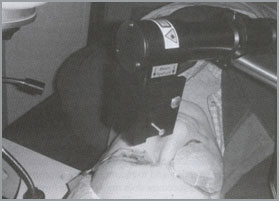
Ultraviolet light exposure
is then carried out using
the Peschke UVX device
(Peschke Meditrade GmbH,
Germany), which is
calibrated to deliver UV
light at 370 nm with an
irradiance of 3mW/cm2 (see
Figure 4). A con¬tact lens
is then placed on the eye as
a bandage and to ensure
comfort, and ciprofloxacin
is instilled. Patients are
instructed to use
ciprofloxacin four times
daily and return the
following 24 to 48 hours to
have the contact lens
removed. Within a few days
an anterior haze is noted,
and this disappears over
time, usually within a few
weeks.
Role in Ectasia
The procedure has been used
with some success in
kerato¬conus and ectasia
following LASIK.
Crosslinking involves the
anterior 300 microns, and
whether ectasia has occurred
because of treatment on form
fruste keratoconus or
through the inadvertent
creation of a thick flap is
not completely rele¬vant, as
both the overlying flap and
stromal bed undergo
crosslinking. The authors
have treated seven eyes with
post¬LASIK ectasia. Data is
hard to interpret based on
small num¬bers and short
follow-up; however, a small
improvement in subjective
visual acuity has been
observed and patients have
reported a decrease in
fluctuation. Of a little
concern is a demonstrable
decrease in central corneal
thickness. This might be
expected because of collagen
fibril thickening and
consequent shortening as
well as transient loss of
keratocytes. Although there
have been reports of
improvements in
ker¬atometry, this has not
been the author's
observation. Overall, the
impression is that the
corneas do stabilize, or at
least the rate of
progression slows
considerably.
Collagen cross linking (CXL)
-
Collagen cross-linking
in the cornea using
riboflavin (B2) - UVA
treatment leads to a
significant increase in
mechanical stiffness of
the corneal Spörl et al
Opthalmologe 1997
-
Increased rigidity by
more than 300%
-
Young’s modulus
increased by 4.5 x
Principle of action CXL
UVA-X
-
Increase in intra- and
inter-fibrillar covalent
bonds by photosensitized
oxidation
-
Penetration of approx.
300 µm
-
Epithelium scraped off
after anesthetic
-
Photosensitizer
riboflavin B2 0.1% in
20% Dextran
-
UVA 370 nm
-
Irradiance 3 mW/cm2 for
30 min
-
Dose of 5.4 J/cm2
-
CL and antibiotic
eye-drops
Side effects
Indications
Keratoconus (KC)
-
Noninflammatory ectasia
of the cornea
-
(Para)central corneal
thinning
-
Irregular astigmatism
-
Bilateral (asymmetric)
and progressive
-
1:2000 in general
population
-
Onset at puberty, 20%
progress to PKP
Management
KC
-
CXL stopped the process
-
23 eyes, follow up
average of 2 years
-
BSCVA better by 1.26
lines in 65%
-
SEQ reduced by 1.14 D
-
Max K post-op progressed
in 1 pt (0.28 D)
-
Pre-op progression of
1.42 D in 52 %
KC
-
Regression!
-
anterior part of the
cornea responsible for
the curvature
-
Max K reduced by 2 D in
70 %
-
Fellow eyes progression
by 1.5 D in 22%
Other degenerations
-
Marginal pellucid
degeneration
-
Keratoglobus
-
Alcali burns
-
Collagenase secretion
from the perilimbal
conjunctiva in the
recovery phase
-
Melting occurs at a
later phase
-
Collagen diseases (SLE,
RA, Polyarteritis
nodosa, Wegener’s
-
granulomatosis,
polychondritis…)
-
Severe persistent
peripheral infiltration
-
Ulceration, thinning and
melting
-
Scleral thinning
Mooren’s ulcer
-
Peripheral ulcerative
keratitis caused by
ischaemic necrosis from
vasculitis of limbal
vessels
-
Adjacent conjunctiva
produces collagenases
and proteglyconases
-
Limited form
-
Unilateral, elderly,
less aggressive
-
Progressive form
-
Bilateral, younger, more
agreesive
Other possibilities
CXL mechanically stabilizes
cornea with KC, keratectasia
or corneal melting
-
More rigid cornea is
more resistant to
collagenases
-
To stop KC progression
at earlier stages
-
To prevent keratectasia
(deeper ablation)
-
To combine with
topo-PRK/EPI/LASEK in KC
forme fruste?
|